Atherosclerosis, a systemic vascular
disease, is a progressive common health problem all over the world1.
This disease may not show any clinical symptoms, but it can be a sign of
serious disease2.
Atherosclerosis is a phenomenon of
dysfunction in the endothelial cells and accumulation of some substances in
tunica intima.3 These substances include lipoprotein particles. They
are foamy macrophage cells resulting from the collection of leukocytes. Thus,
smooth muscle cells in the tunica media begin to form atheroma plaques4,5.
This may lead to both cardiovascular disease and pseudoexfoliation syndrome6.
Ocular pseudoexfoliation (PEX) is the
detection of fibrillar extracellular matrix accumulation on the anterior
segment of the lens, pupil circumference, iris epithelium or zonules during the
anterior segment examination7. The mechanism and the etiology of PEX
formation has not been fully understood. Furthermore, the relationship of ocular
PEX with systemic diseases has been demonstrated in various studies8-14.
Many diseases can be diagnosed early with
internal carotid artery intima media thickness (CAIMT).9
Ultrasonography technique is an inexpensive, easy and non-invasive method
through which intima media thickness is measured10. Many studies
have been conducted to measure intima media thickness in diabetics, obesity,
and renal failure patients and dyslipidemia11,12.
The aim of this study is to compare the internal
carotid artery intima-media thickness (CAIMT) in patients with ocular PEX and
healthy individuals, and to show that ocular PEX may be related to systemic
diseases such as atherosclerosis, or not.
MATERIAL AND METHODS
Our study was a cross-sectional clinical
study which included 32 patients with or without ocular PEX (40-80 years of
age) who were admitted to the Department of Ophthalmology in Adana Ortadogu Hospital
between January 2017 and January 2018. The patients were admitted to our clinic
with the complaint of low vision. The ethical approval was obtained from the
ethics committee of Adana City Hospital in Adana in Turkey and informed consent
was obtained from the all participants.
In the biomicroscopic anterior segment
examination, 16 patients were diagnosed with pseudoexfoliative material on the
pupil margin or anterior lens capsule. These patients formed the first group
(Group I). Other 16 non-PEX patients were accepted as a control group (Group
II). Patients with systemic disease such as hypertension, diabetes mellitus
were excluded from the study.
CAIMT was measured and noted in all participants.
Carotid artery Doppler USG was used to measure CAIMT. The data was compared by
statistical analysis. Mean, standard deviation, median lowest, highest,
frequency and ratio values were used in descriptive statistics of the data. The
distribution of the variables was measured with the Kolmogorov-Simirnov Test.
Independent Sample T Test was used to analyze the quantitative independent
data. χ² test was used for the comparison of normally distributed
categorical variables. SPSS 22.0 program was used in the analysis.
RESULTS
The demographic variables of the sample are presented
in Table 1. In Group I and Group II, the age of the patients did not differ
significantly (p > 0.05). In Group I and Group II, gender distribution was
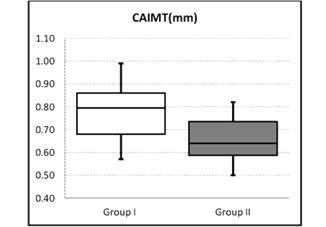
not significant (p > 0.05). In Group I, CAIMT was significantly higher than in
Group II (p < 0.05) (table 2 and figure 1).
Table
1: Demographic variables of the sample.
|
|
|
Min-Max
|
Median
|
Mean ± SD/N%
|
|
Age
|
|
43.0 – 78.0
|
64.0
|
61.2 ± 9.7
|
|
Sex
|
Male
Female
|
|
|
16
16
|
50%
50%
|
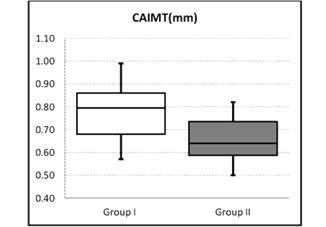
Fig. 1: The comparison of CAIMT between the groups.
DISCUSSION
Pseudoexfoliation syndrome (PEXS) is a
clinically diagnosed disease and its etiopathogenesis has not been determined
yet. However, there are studies showing that there is a relationship between
PEXS and systemic diseases. In addition, PEX is a common age-related systemic
metabolic vascular disease affecting the elastin microfibrillar tissue. It is
characterized by white grey extracellular flaky material in the anterior
segment.15According to microscopic findings, PEX materials have been
found in blood vessel wall, which could affect the function and elasticity of
blood vessels, as shown by increased carotid artery stiffness16 and
reduced brachial artery endothelial cell function17.
Schumacher et al. reported that five ocular
PEX patients who were sampled from the aortic artery had significant PEX
accumulation in the vessel intima media9. Cahill et al. conducted
another study which demonstrated the systemic involvement of PEX. They showed
the deposition of fibrilsin in the tectorial membrane of the inner ear.
Bilateral sensorineural hearing loss was observed in the majority of patients
with PEX, regardless of age and glaucoma18.
In a study in which the relationship
between PEX and diabetes mellitus was investigated, there was no relationship
between PEX and diabetes. In this study PEX ethiopathogenesis was attributed to
genetic and biochemical factors14. In a study by Ekström et al, the
relationship between PEXS and aortic aneurysm was investigated, but no
association was found between the two diseases19,20.
Increased arterial wall thickness and
changes in the vascular structure, expressed as CAIMT, have been identified as
predictors of unexpected cardiovascular events. CAIMT has been shown to be an
early marker of endothelial tissue damage and an early sign of atherosclerotic
vascular disease21,22.
CAIMT is highly correlated with the presence of
coronary pathology and myocardial infarction. Carotid disease is seen in 30-60%
of people with peripheral vascular disease. Approximately 50-60% of patients
with carotid disease have advanced coronary disease, while only 10% of patients
with coronary artery disease have advanced carotid disease23.
Therefore, we believe that early detection of increased CAIMT will have an
important role in prevention of cardiological and neurological diseases.
CONCLUSION
There is a positive link between CAIMT and ocular PEX
in our study. Since CAIMT is associated with atherosclerosis, there may also be
an association between ocular PEX and atherosclerosis. In this context, with a
simple eye examination, it can be learned whether the patients have a risk of
coronary artery disease, or not. This may also help in the early diagnosis of
atherosclerosis. However, future studies pointing this subject are needed to
clarify these findings.
Conflict of Interests
All authors declare that they have no conflict of interests.
Author’s Affiliation
Oguz Guvenmez, MD
Special Internal Medicine Clinic, Adana, Turkey.
Asim Kayiklik, MD
Department of Ophthalmology, Adana Ortadogu Hospital,
Adana, Turkey.
Author’s contribution
Oguz Guvenmez, MD
Study Design, interpreting results, writing manuscript.
Asim Kayiklik, MD
Collecting data, Statistical analysis, writing
manuscript.
REFERENCES
1. Ross
R. Atherosclerosis. In: McGee J, Isaacson PG, Wright NA, editors. Oxford
Textbook of Pathology. Vol. 2, Oxford: Oxford University Press; 1992: 798-812.
2. McGill
HC Jr, McMahan CA. Determinants of atherosclerosis in the young.
Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group.
Am J Cardiol. 1998; 82: 30-6.
3. Rafieian-Kopaei
M, Setorki M, Doudi M, Baradaran A, Nasri H. Atherosclerosis: process,
indicators, risk factors and new hopes.Int J Prev Med. 2014; 5: 927-46.
4. Kuller
L, Borhani N, Furberg C, Gardin J, Manolio T, O’Leary D, et al. Prevalence
of subclinical atherosclerosis and cardiovascular disease and association with
risk factors in the Cardiovascular Health Study. Am J Epidemiol. 1994; 139:
1164-79.
5. Touboul
PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al.
Mannheim carotid intima-media thickness consensus (2004-2006). An update on
behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium,
13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and
Brussels, Belgium, 2006. Cerebrovasc Dis. 2007; 23: 75-80.
6. Siordia
JA, Franco J, Golden TR, Dar B. Ocular pseudoexfoliation syndrome linkage
to cardiovascular disease. Curr Cardiol Rep. 2016; 18: 61.
7. Küchle
M, Amberg A, Martus P, Nguyen NX, Naumann GO. Pseudoexfoliation syndrome
and secondary cataract. Br J Ophthalmol. 1997; 81: 862-6.
8. Shrum
KR, Hattenhauer MG, Hodge D. Cardiovascular and cerebrovascular mortality
associated with ocular pseudoexfoliation. Am J Ophthalmol. 2000; 129: 83-6.
9. Su
TC, Chien KL, Jeng JS, Chen MF, Hsu HC, Torng PL, et al. Age - and
gender-associated determinants of carotid intima-media thickness: A
community-based study. J Atheroscler Thromb. 2012; 19: 872–80.
10. Jaroch
J, Loboz Grudzien K, Bociaga Z, Kowalska A, Kruszynska E, Wilczynska M, et al.
The relationship of carotid arterial stiffness to left ventricular diastolic
dysfunction in untreated hypertension. Kardiol Pol. 2012; 70: 223–31.
11. Takiuchi
S, Rakugi H, Fujii H, Kamide K, Horio T, Nakatani S, et al. Carotid
intima-media thickness is correlated with impairment of coronary flow reserve
in hypertensive patients without coronary artery disease. Hypertens Res. 2003; 26:
945–51.
12. Schumacher
S, Schlötzer-Schrehardt U, Martus P, Lang W, Naumann GO. Pseudoexfoliation
syndrome and aneurysms of the abdominal aorta. The Lancet, 2001; 3: 357: 359-60.
13. Rinvold
A. Pseudoexfoliation and aortic aneurysms. The Lancet, 2001; 357: 2139.
14. Psilas
KG, Stefaniotou MJ, Aspiotis MB. Pseudoexfoliation syndrome and diabetes
mellitus. Acta Ophthalmol (Copenh), 1991; 69: 664-6.
15. Streeten
B, Gibson S, Dark A. Pseudoexfoliative material contains an elastic
microfibrillar-associated glycoprotein. Trans Am Ophthalmol Soc. 1986; 84: 304-20.
16. Visontai
Z, Merisch B, Kollai M, Holló G. Increase of carotid artery stiffness and
decrease of baroreflex sensitivity in exfoliation syndrome and glaucoma. Br J
Ophthalmol. 2006; 90: 563.
17. Naji
M, Naji F, Suran D, Gracner T, Kanic V, Pahor D. Systemic endothelial
dysfunction in patients with pseudoexfoliation syndrome. Klin Monbl Augenheilkd,
2008; 225: 963-7.
18. Cahill
M, Early A, Stack S, Blayney AW, Eustace P. Pseudoexfoliation and
sensorineural hearing loss. Eye, 2002; 16: 261-6.
19. Ekström
C, Wilger S, Wanhainen A. Pseudoexfoliation and aortic aneurysm: a
long-term follow-up study. Acta Ophthalmol. 2019; 97 (1): 80-83.
20. Besir
FH, Yazgan S, Celbek G, Aydın M, Yazgan Ö, Erkan ME, et al. Normal
values correlates of carotid intima-media thickness and affecting parameters in
healthy adults. Anadolu Kardiyol Derg. 2012; 12: 427-33.
21. Mayet
J. Is carotid artery intima-media thickenning a reliable marker of early
atherosclerosis? J Cardiovasc Risk, 2002; 9: 77-81.
22. Jadhav
UM. Carotid intima media thickness as an independent predictor of coronary
artery disease. Indian Heart J. 2001; 53: 458-62.
23. Magyar
MT, Szikszai Z, Balla J, Valikovics A, Kappelmayer J, Imre S. Early – onset
carotid atherosclerosis is associated with increased intima – media thickness
and elevated serum levels of inflammatory markers. Stroke, 2003; 34: 58-63.